Estimated reading time: 12–15 minutes • Buyer’s guide + safe‑use playbook inside
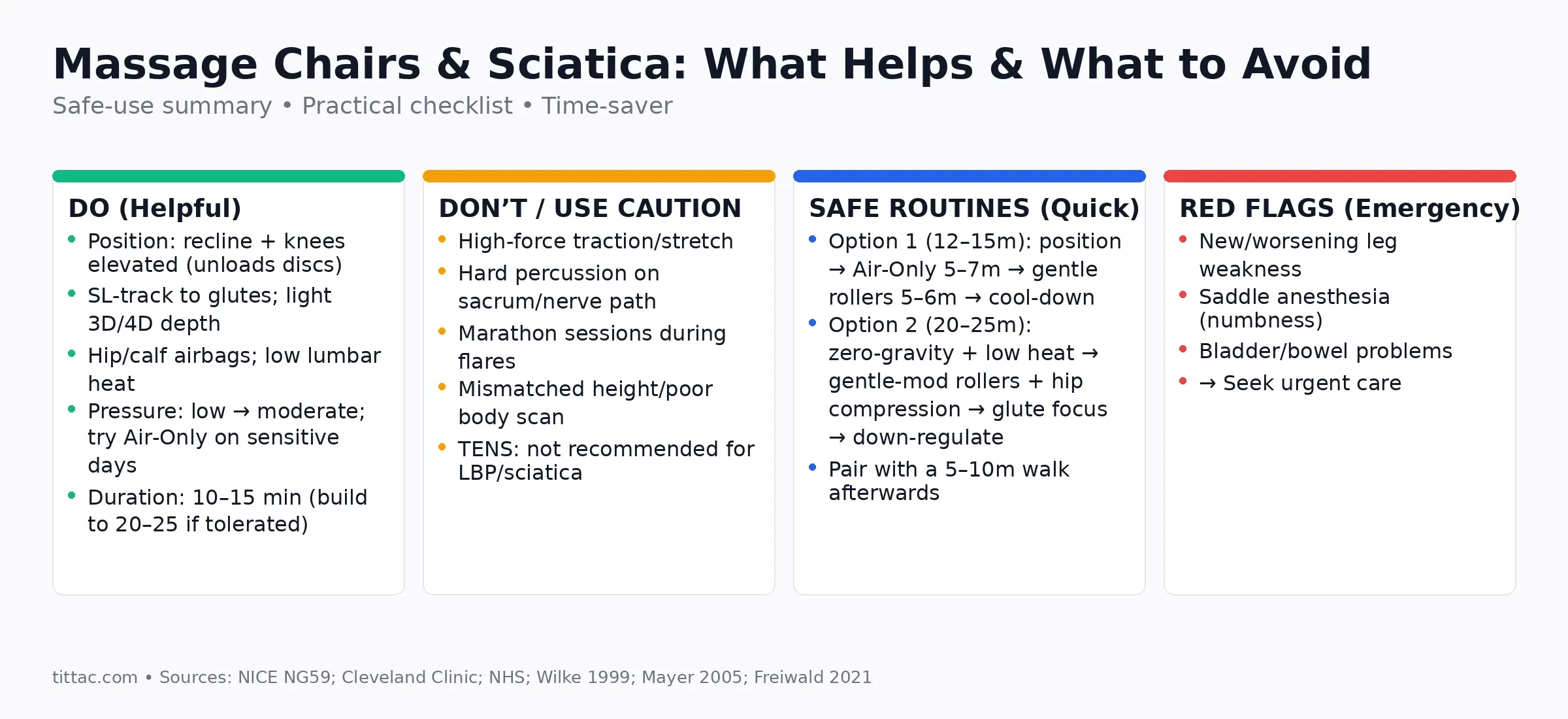
Looking for a massage chair for sciatica? This guide explains what actually helps (SL‑track glute coverage, adjustable 3D/4D depth, gentle hip/calf air compression, low lumbar heat, and knees‑elevated recline) and what to treat with caution (high‑force traction, aggressive percussion, marathon sessions). You’ll also find two safe starter routines, a quick buyer’s checklist, and clear flags for when to seek medical care. Use this as a practical roadmap to reduce discomfort, stay moving, and choose a chair that fits your body and space.
Table of Contents
Key takeaways (TL;DR)
- Sciatica = irritation or compression of the sciatic nerve, usually causing pain that radiates down one leg (sometimes with tingling, numbness, or weakness). Most cases improve with time and self‑care; severe or persistent symptoms need clinical assessment [2][3].
- Massage chairs can help some people by easing muscle guarding and improving comfort, but they’re best used as part of a broader plan (keep moving, do appropriate exercise, and self‑manage). Guidelines support manual therapy only as part of a package that includes exercise [1].
- Helpful chair features: gentle adjustable rollers (2D/3D/4D), SL‑track coverage into the glutes, air compression for hips/calves, lumbar heat, and recline with knees slightly elevated (“zero‑gravity”) [5].
- Use caution or avoid: high‑force “traction/stretch” routines, aggressive percussion on the sacrum or along the nerve path, one‑size programs that don’t fit your height, and marathon sessions during an acute flare. Traction and TENS are not recommended for sciatica [1].
- Low, steady lumbar heat can provide short‑term pain relief and comfort in acute low‑back pain phases, which may help people with sciatica tolerate movement better [6][7].
What is sciatica—and why chairs can (sometimes) help
Sciatica refers to symptoms caused by irritation, inflammation, or compression of the sciatic nerve—the large nerve running from your lower back through the buttock and down the back of your leg. It’s commonly triggered by a herniated disc, bony narrowing (spinal stenosis), or other compression. Most cases improve over time with conservative measures [2].
Massage chairs can’t “fix” the root cause (for example, shrink a disc), but they may reduce muscle guarding, ease perceived tension, and improve comfort—often enough to help you move more, which is central to recovery in many cases. Current guidance recommends manual therapy (including soft‑tissue techniques like massage) only as part of a treatment package that includes exercise (and sometimes a cognitive‑behavioral approach) [1].
When to seek urgent care: new or worsening leg weakness, numbness in the inner thighs/saddle area, or loss of bladder/bowel control can indicate cauda equina syndrome—a medical emergency. Get help immediately [3][4].
The biomechanics: why “zero‑gravity”‑style positioning feels good
“Zero‑gravity” recline elevates your knees and gently opens the hips. In vivo research measuring lumbar intradiscal pressure across positions shows lower pressures in supine postures, and particularly that lying supine with knees flexed returns disc pressure to a low baseline compared with straightened legs. That unloading is one reason many people with sciatica feel relief in reclined, knees‑elevated positions [5].
Features that genuinely help (and how to use them)
SL‑track rollers that reach the glutes
Sciatica often involves protective tightness in the deep hip rotators (e.g., piriformis) and gluteal tissues along the nerve’s path. SL‑track rollers follow the spine and sweep into the seat, contacting the glutes and upper hamstrings without jabbing the lumbar spine. Prioritize accurate body‑scan calibration, gentle starting depth, and the option to spot‑massage the buttock (avoid direct pounding over the sacrum). Remember: manual therapy (including massage) is most effective when paired with movement/exercise, not used alone [1].
Air compression for hips, thighs, and calves
Airbags provide rhythmic squeeze‑and‑release that many find soothing when rollers feel too intense. Light hip/thigh compression can calm surrounding tissues; calf compression and foot rollers help ease lower‑leg fatigue, which can accumulate as you increase walking—often a useful activity in recovery. Keep the pressure comfortable and avoid numbness/tingling.
Lumbar heat (low, steady warmth)
Heat therapy has short‑term benefits for acute low‑back pain: randomized trials and reviews show continuous low‑level heat can reduce pain and improve function, which helps many people tolerate gentle activity. In a chair, choose low–medium heat and avoid prolonged high heat on areas with reduced sensation [6][7].
Recline and leg‑elevation control
Micro‑adjusting recline and leg height lets you find the “sweet spot” where your back feels light. This aligns with disc‑pressure data showing that knees flexed/elevated reduces intradiscal load compared with legs straight. Start near a zero‑gravity preset, then fine‑tune [5].
Fine‑grained intensity and speed control (2D/3D/4D)
Symptoms fluctuate. On flare days, even premium 4D rollers can feel too strong at high depth. Look for low starting intensity, adjustable width and speed, and programs that let you switch to air‑only. Comfort and control matter more than spec sheets.
Settings and programs to avoid (or use carefully)
Spinal stretch/traction claims
Some chairs market “traction” or intense passive “stretch.” Major guidelines recommend not offering traction for low‑back pain with or without sciatica. If your chair has a stretch routine, treat it as gentle mobility only; stop if symptoms worsen or travel further down the leg [1].
Aggressive percussive pounding over the sacrum or along the nerve path
Direct, high‑force percussion on the sacrum or posterior thigh can irritate sensitized tissues. Save percussive modes for upper‑back areas or skip them during flares.
One‑size‑fits‑all programs that don’t match your height
Poor scans lead to rollers hitting bone instead of muscle. Always run the body scan, confirm shoulder position markers, and adjust manually if needed.
Marathon sessions during acute flares
Long, intense sessions can ramp up sensitivity. Early on, think short and frequent, not long and punishing.
Electro‑stimulation/TENS accessories
Some chairs or add‑ons promote TENS. Guidance says do not offer TENS for low‑back pain with or without sciatica because evidence of benefit is lacking [1].
A safe starter routine (2 options you can try today)
Stop if pain worsens, radiates further, or if you feel spreading weakness/numbness. When in doubt, consult a clinician.
Option 1: 12–15 minutes (flare‑friendly)
- Positioning (2 min): Recline to a knees‑elevated posture; low lumbar heat on [5].
- Air only (5–7 min): Gentle hip/thigh compression + light calf squeeze.
- Gentle rollers (5–6 min): Low depth, slow speed over lower back and glutes. Avoid percussion.
- Cool‑down (1–2 min): Rollers off; keep heat if soothing.
Frequency: 1–2×/day as tolerated. Pair with a short walk (5–10 minutes) afterward to keep you moving—often part of supportive sciatica care [8].
Option 2: 20–25 minutes (settling phase)
- Positioning (3 min): Zero‑gravity style; lumbar heat on low–medium [5].
- Mixed mode (10–12 min): Low–moderate rollers across low back → glutes; intermittent hip compression.
- Focused glutes (5–6 min): Spot massage on the buttock (avoid direct sacrum).
- Down‑regulate (2–3 min): Air‑only + slow breathing.
Choosing the right chair for sciatica: a quick buyer’s checklist
- Fit & scan: Height range covers you; shoulder markers align; scan is accurate and repeatable.
- Roller system & track: SL‑track coverage into the glutes; adjustable depth (3D/4D); manual spot + width control.
- Comfort controls: Independent leg elevation; low/medium lumbar heat; adjustable hip/thigh/calf airbags; quiet operation [6].
- Programs: Lower‑back + glute sequences; “air‑only” days; gentle “stretch” (avoid high‑force traction) [1].
- Practicalities: Space‑saving recline; solid warranty; white‑glove delivery if doorways/stairs are tricky.
What a massage chair can—and can’t—do for sciatica
Can do: ease muscle guarding in the lumbar/glute region, provide temporary pain relief and relaxation so you can move more, support a consistent self‑care routine (heat + gentle pressure), and sometimes improve sleep comfort.
Common mistakes to avoid
- “More pressure must be better.” With nerve‑related pain, tolerance beats force. Start gentle; increase only if relief lasts beyond the session.
- Pounding the symptoms. Avoid direct high‑force percussion on the sacrum/posterior thigh.
- Skipping the body scan. Misaligned rollers jab bone instead of muscle; recalibrate every time a different user sits down.
- Too‑hot heat. Choose low–steady warmth; prolonged high heat—especially on areas with reduced sensation—isn’t wise [7].
- Relying on traction/TENS to “fix it.” Traction and TENS are not recommended for sciatica; treat any “stretch” program as light mobility only [1].
Pairing your chair with the rest of your plan
- Keep moving: Continue normal activities and add gentle exercise as able; walking is commonly used [1][8].
- Build consistency: 10–20 minutes of chair time plus a short walk often beats sporadic long sessions.
- Track what helps: Favor positions/programs that reduce leg symptoms (not just back tension).
- Know when imaging helps: Imaging is not routinely recommended early for sciatica unless results are likely to change management [1].
- Work with a clinician: Especially if symptoms persist beyond a few weeks, or if you’re unsure which exercises are appropriate for your situation [1].
Helpful vs. unhelpful: a quick comparison
| Often helpful | Often unhelpful / use caution |
|---|---|
| Reclined, knees‑elevated position (unloads lumbar discs) | Long periods of deep forward flexion or slumped sitting |
| SL‑track rollers with gentle depth; glute coverage | High‑force percussion over sacrum/along nerve path |
| Air compression at hips/calves; “air‑only” programs on sensitive days | Over‑tight compression causing tingling/numbness |
| Low‑level lumbar heat for short‑term relief | Prolonged high heat on areas with reduced sensation |
| Short, frequent sessions that leave you more willing to move | Marathon sessions during acute flares |
| Manual therapy as part of a package with exercise | Relying on passive modalities alone; traction/TENS to “fix discs” |
Why: Disc‑pressure data support knees‑flexed/reclined positioning; heat has short‑term benefits in acute low‑back pain; guidelines prioritize activity and caution against traction/TENS for sciatica [5][7][1].
FAQs
Will a massage chair cure my sciatica?
No. It can help manage symptoms and comfort so you can be more active—a key part of recovery for many. Severe or persistent cases need clinical assessment [2].
Is heat safe for sciatica?
For many people, low, steady lumbar heat is soothing and supported for short‑term relief in acute low‑back pain. Keep settings modest and avoid prolonged high heat, especially on numb areas [6][7].
What about a chair’s “stretch/traction” mode?
Treat it as gentle mobility only. Traction is not recommended for low‑back pain with or without sciatica. Stop if symptoms worsen or travel further down the leg [1].
How long should a session be?
Start with 10–15 minutes at low intensity. If you feel better afterward (and the benefit lasts), build toward 20–25 minutes. If soreness lingers more than a couple of hours, scale back next time.
Do I need a 4D chair?
Not necessarily. What matters is fit, scan accuracy, and the ability to go very gentle on flare days. A well‑tuned 2D/3D chair with SL coverage can work well.
When should I seek urgent care?
Red‑flag symptoms like new/worsening leg weakness, saddle numbness, or bladder/bowel problems need immediate attention [3][4].
Final word
A massage chair can be a useful tool for managing sciatica—especially when you prioritize fit, gentle adjustability, SL‑track glute coverage, air compression, and low‑level heat. But the best outcomes come when you pair the chair with movement, simple education, and time. If symptoms are severe, worsening, or not improving in a reasonable window, see a healthcare professional to tailor a plan to your specific cause of sciatica [1][2].
Sources & further reading
- NICE Guideline NG59: Low back pain and sciatica in over 16s: assessment and management ↩
- Cleveland Clinic: Sciatica — What It Is, Causes, Symptoms, Treatment & Pain Relief ↩
- NHS: Sciatica ↩
- Cleveland Clinic: Cauda Equina Syndrome ↩
- Wilke H‑J, et al. New In Vivo Measurements of Pressures in the Intervertebral Disc in Daily Life (1999). ↩
- Mayer JM, et al. Treating Acute Low Back Pain with Continuous Low‑Level Heat Wrap Therapy and/or Exercise: A Randomized Controlled Trial (2005). ↩
- Freiwald J, et al. A Role for Superficial Heat Therapy in the Management of Non‑Specific Low Back Pain (2021 review). ↩
- Cleveland Clinic Abu Dhabi: Sciatica ↩